
A History of Our COVID-19 Precautions
It was almost two years ago that we started taking precautions against the spread of COVID-19. During the second half of February 2020, we were told not to touch surfaces, and we discovered how often we touch our faces.
By the middle of March 2020, I was worried massage therapy schools and massage therapy centers would be important vectors of infection. The biggest risk factors seemed to be proximity and time, and there is no way to do – or teach – massage without large doses of both. I was not sure there was a future for our profession. I could visualize the headlines about a massage therapist having spread the disease to 20 clients, or a Massage Envy being the epicenter of an outbreak affecting hundreds. I could picture an article about thousands of these incidents.
That didn’t happen. Certainly, COVID- 19 has spread in massage treatment rooms, and schools. I know of several cases of each. In each case though, at least one guideline was ignored, or followed incorrectly. And those cases have not been the big story; the spotlight instead is on bars, restaurants, and large indoor gatherings. Massage therapy schools and offices are relatively safe when reasonable public health guidelines are followed.
19 has spread in massage treatment rooms, and schools. I know of several cases of each. In each case though, at least one guideline was ignored, or followed incorrectly. And those cases have not been the big story; the spotlight instead is on bars, restaurants, and large indoor gatherings. Massage therapy schools and offices are relatively safe when reasonable public health guidelines are followed.
The precautions recommended by public health professionals have regularly changed over the past two years, and everyone on the planet has made choices about which ones to follow. It has sometimes been difficult to navigate the information tsunami, and figure out what best applies to a massage therapy school or practice. If you want the Cliffs notes, it’s simple: well-fitting masks, ventilation, and filtration. If you live somewhere that it’s legal and practical, add boosted vaccination to that list. If you want the details, read on.
Before suspending live classes on March 13, 2020, Sarasota School of Massage Therapy (SSMT) spent several weeks acting on the best information available. That this information turned out to be woefully inadequate was counterbalanced by the relatively low numbers of infections in the community. It’s not that spraying Lysol everywhere, washing our hands constantly, and avoiding putting our hands on our faces worked – it’s that no one brought the virus into the school to test our procedures.
Over the next six months we conducted science and theory classes online, and did not return to the classroom until the Florida 2020 summer wave had abated. During those months in school purgatory, an enormous body of research was published, and thankfully, provided without a paywall. One of the bright spots during this pandemic has been the ready accessibility of everything published by The Lancet, The New England Journal of Medicine, BMJ (formerly British Journal of Medicine), the Journal of the American Medical Association, Science, and others. The world owes a debt of gratitude to these journals for keeping us informed. Their annual subscription fees are usually more than $150 each, and individual articles can cost $40 or more.
The procedures recommended by epidemiologists based on research published in these journals has changed slightly since SSMT resumed classroom instruction in September 2020, but the basic outlines have not. We credit those safety procedures for having prevented the transmission of COVID-19 in our school for nearly the past year and a half, through three large surges, including the latest Omicron wave, which has infected about 40% of Americans, and is likely to infect another 20% before the end of March.
Since September 2020, 16 people have entered the school building during their most infectious period, unknowingly infected with SARS-CoV-2, hours before developing symptoms. They spent five hours in a classroom, with classmates and instructors, breathing in the same room, and often with a classmate practicing massage between one and five feet from their noses. That’s over 150 people, and over 7,000 people-hours of CDC-defined close contact, and not a single known transmission. Well- maybe one, but I doubt it.
In each case of exposure, we sent those exposed to a 14 day quarantine (recently decreased to ten days), and each quarantined person submitted PCR results from a swab taken on Day 5 (occasionally later). None of the over 150 people quarantined developed symptoms. While one tested positive, that person was likely exposed to infection elsewhere in the community.
Each of the safety procedures discussed below is imperfect. We knew from the beginning that some were likely more useful than others. Each is considered a piece in a larger system; the Swiss cheese model. If virions escaped a mask, they would also have to escape a variety of air purification and ventilation systems to get into a respiratory tract. As far as we know, not enough of them did so to cause infection.
Face Coverings
When we first returned to the classroom in September 2020, we required everyone in the building to wear a mask. The mask needed to either be a school-supplied ASTM Level 3 surgical mask, or a multi-ply cotton, or cotton/poly blend. All masks needed to have a nose-wire, and be as well sealed as possible all around.
Surgical masks come with different ratings. At the bottom of the scale are the unrated surgical-mask-look-a-likes: blue paper masks meant to protect from dust. These offer little protection from SARS-CoV-2. An SSMT graduate caught the disease from her client while both were wearing these.
Next come PM 2.5 rated masks. These are considered medical grade, and are often used in hospitals – but not in COVID wards. The 2.5 in the rating means they have been tested to filter out particles down to 2.5 microns. Many virus-containing droplets can be filtered out by these masks, but others are ten times smaller.
ASTM Level 2 and Level 3 masks filter out over 98% of droplets down to .3 microns. This is the “magic number” at which all medical grade masks, including N-95’s, are tested. The most difficult particle size to filter is .3 microns, until you get much smaller. Particles at .1 micron tend to zig-zag, a characteristic known as Brownian motion, so they get trapped more easily. A mask that can filter over 98% of particles at .3 microns does even better with particles both larger and smaller – though Oxygen and Carbon dioxide molecules, which are over 1,000 times smaller, are not filtered.
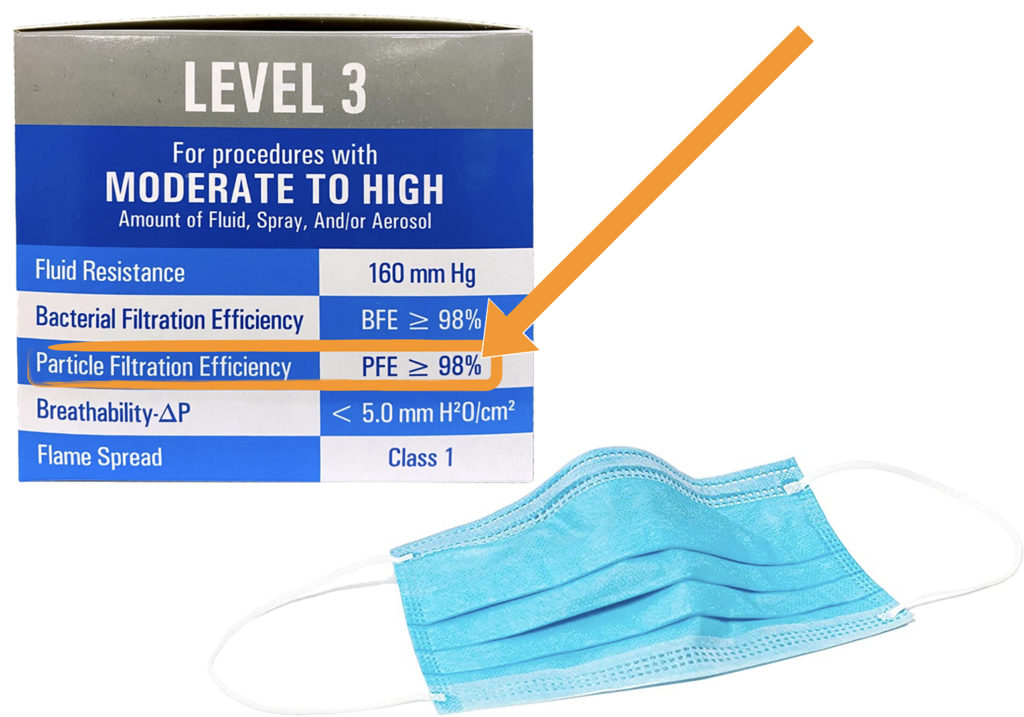
ASTM Level 2 and Level 3 masks have identical ratings for aerosol filtration; their difference is in liquid filtration capacity, against blood borne pathogens. We use Level 3, but you really could just as well spend less, and use Level 2.
The problem with surgical masks, or cloth masks with a surgical filter in a pocket, is not their filtration capacity, it’s leakage. Even the best fitting Level 3 mask leaks around the edges.
A fit-tested and seal-tested N-95 mask doesn’t leak. The problem with N-95’s for the general population is it is rather difficult to get a proper fit and seal. An ill-sealed N-95 can leak even more than a surgical mask. N-95 masks create greater resistance, making it more difficult to breathe, and forcing any exchanged air to more readily take the path of least resistance – through the leak. If you know how to fit and seal-test an N-95 it is by far the best choice – if you don’t, you are probably better off with a Level 3 surgical mask hacked to improve its fit by tying the ear-loops, tucking the pleats, and tying the back around the head instead of the ears. Double-masking also decreases leakage.
The way most people wear them, a surgical or multi-ply cotton mask decreases the risk of the wearer by about 50%. A mask on an infected source protects those around them by more than four times. The combination of masks on the source and the target decreases the virus exchanged more than 8-fold. 2 hours of contact between two well-masked people is likely safer than 15 minutes between two un-masked people at the same distance.
In addition to a well-fitting mask, we initially required students to wear a school-supplied face-shield that sits on the base of the neck/shoulder girdle. Many epidemiologists were recommending these as an adjunct to masks. Any large particles that got around an imperfectly fitting mask would be blocked by the shield. A shield alone would fail to prevent the buildup of aerosols in the room – the mask was for that.
Over the past 18 months our face-covering requirements have changed several times. It became clear aerosols were the problem, and shields were not particularly helpful. We went to double masking, and then to single-masking for the fully vaccinated. In the spring of 2021, when the data showed fully vaccinated people to be well protected against infection, in addition to symptomatic disease – and the community was experiencing a relative lull in infections – we allowed the vaccinated to go mask-less. When the Delta variant broke through that protection to an extent, we reverted to masks for all.
We eventually moved to require school-supplied ASTM Level 3 surgical masks for all. We realized it was too difficult to know what everyone’s cloth mask was made from, and whether or not there was a surgical grade filter in its pocket.
Ventilation and Air Purification
COVID-19 is a disease mostly transmitted through indoor air. Transmission is possible at crowded outdoor events, and theoretically possible (but vanishingly rare) from surfaces, but the vast majority of people catch COVID-19 breathing indoor air.
When SSMT resumed on-campus classes in September 2020, neither the CDC nor the WHO had acknowledged the aerosolized nature of the virus, though there was an increasing call from epidemiologists for them to do so.

There was enough evidence from early in 2020 (the restaurant AC-mediated infections in Wuhan, the choir practice in Washington state in which a single infected singer likely passed the virus to 52 out of 60 others in the room, etc.) We took the advice of the epidemiologists who wrote an editorial in JAMA in May 2020 suggesting the use of HEPA filters in all public indoor air spaces. We purchased units for every classroom, corridor, bathroom, and office; enough to achieve at least six air changes per hour. When the Delta variant was found to increase the amount of virus shed, we bought additional units bringing the air changes up to 7-9 per hour. We like Levoit filters for their combination of clean air delivery rate, quiet, and value. Blue-Air and others also get good reviews.
When we designed our facility, we put recessed hydrocollator bays in each classroom, with exhaust fans that vented through the roof. The idea was to prevent the buildup of moist hot air in our Florida classrooms every time someone opened a hydrocollator. These can be turned on and off with a switch, when someone opens a hydrocollator. During the pandemic, we have left them always on, and poked another hole in the building to bring fresh outside air into the corridor through a duct. The air vented to the outside through the hydrocollator vents creates a negative pressure, drawing fresh air in from the corridor, under the door. This add another 1.3 air changes per hour – and helps decrease carbon dioxide levels, which HEPA filtration does not.

In the spring of 2021 we ordered openable windows to replace existing windows. Those finally arrived and were installed in December. We leave those open even when the weather is unpleasant, and compensate with additional heat or air conditioning.
Open windows – and ducts bringing outside air directly in – are inefficient means of ventilation. We will be looking at a heat pump, to exchange indoor and outdoor air without bringing 95˚ summer air or 45˚ winter air into the classrooms.
That there hasn’t been a national movement to subsidize the installation of heat pumps and HEPA filters in public indoor environments boggles my mind. We ask people to wear masks, but we don’t ask businesses to clean up the air their customers breathe. We spent trillions to stay home in the spring of 2020, and spend more money every time people are isolated, quarantined or hospitalized, but it hasn’t occurred to us to support a preventative measure with a long-term benefit, that requires nothing of the public.

We also put UV-C units in our five HVAC units. This was rather expensive, as we bought the best units we could find, and I am not convinced they make much difference.
The germicidal UV-C units used in hospitals draw air through a long tubular duct filled with UV-C light. The small time air in a commercial HVAC unit passes by a UV-C lamp pales in comparison. A few pathogens are probably killed, but if I had to choose one of our ventilation/purification methods to skip, it would be this one; in terms of cost /benefit calculus, it comes up the weakest.
Disinfection
We have always wiped down surfaces with a germicidal agent. When we resumed live classes in September 2020, we expanded the list of surfaces and moved to a twice daily disinfection of all surfaces. We continue to do this mostly because it is appropriate infection control, though we understand it is more likely to prevent MRSA, flu, and other pathogens, than it is to affect COVID transmission.
COVID-specific disinfection is largely hygiene theater, and can be more damaging than helpful. Spending ten minutes packed into an unventilated, unfiltered jetway, waiting to board an airplane, only to be given a disinfecting wipe by the flight attendant at the threshold is a great example of the destructive distraction that is hygiene theater. There is nothing wrong with the wipe per se; it is just the mistaken sense you have done something useful, while ignoring the important things that need to be done.
Despite the length of this piece, those things are simple. Deal with breathing, using masks, ventilation, and filtration. Pay attention to the quality of each. Use N95’s if you are confident in fit and seal; ASTM Level 2 or 3 otherwise, with the pleats tucked, and ear-loops tied at the mask, and clasped on the back of the head. Ventilate as much as you can manage. Filter indoor air with HEPA filtration, with at least six air changes per hour.
Of these, the first to go may be masks. It is certainly premature to be dropping them now, as many states are doing, while Omicron is still rampant. We still have no data on the risk of Long COVID from Omicron, and the risk of spreading this potentially debilitating disease in a classroom, when masking dramatically reduces the risk, makes dropping them now a mistake. That calculus may change sometime in March or April, and it may not.
I see no reason for ventilation/HEPA filters to end, and hope if there are any permanent changes we make because of the pandemic, it will be a permanent improvement to the quality of indoor air.
Dozens of SSMT students, instructors, clinic clients and staff have contracted COVID-19 during the past two years, but they all caught it outside our facility. One of those students died. It breaks my heart to picture her face, and realize her death was entirely preventable. If she had followed the procedures we follow at SSMT in the rest of her life, and if she had been vaccinated, she would almost certainly be alive today.
Amidst all the conflicting and changing guidance, what has been clear all along is this is a disease transmitted through public indoor air. Masks, ventilation, and HEPA filters, along with proper screening, quarantine, and isolation protocols, have proven effective at prevention. None of these measures are perfect, and someone might yet contract the disease on our campus (there is a chance someone already has).
When a student calls in and says “I just woke up with a fever, and the feeling of an elephant on my chest, and I was in class last night,” they are sent for a PCR test, and their class, and any exposed instructors are sent home for quarantine. When no one else develops symptoms, and when all those exposed test negative by PCR, and when this happens again and again, we figure we have found a way to responsibly run a massage therapy school during the COVID-19 pandemic.
